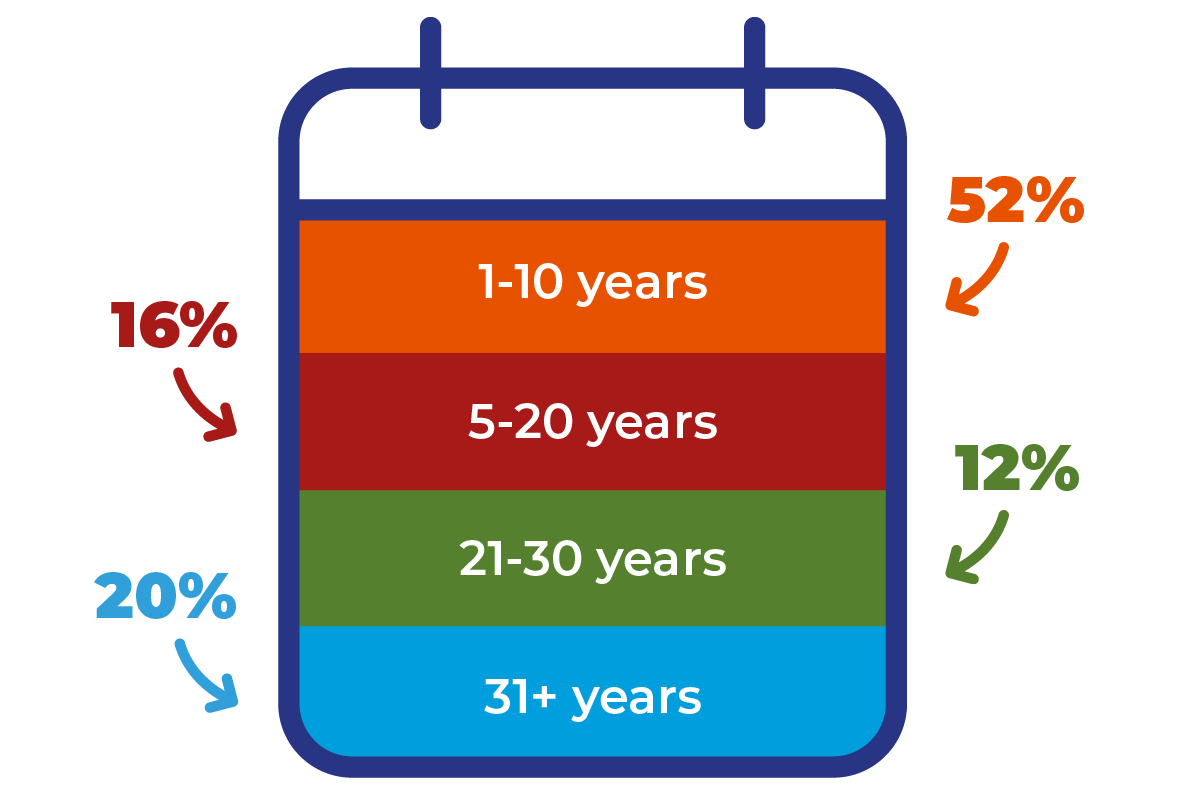
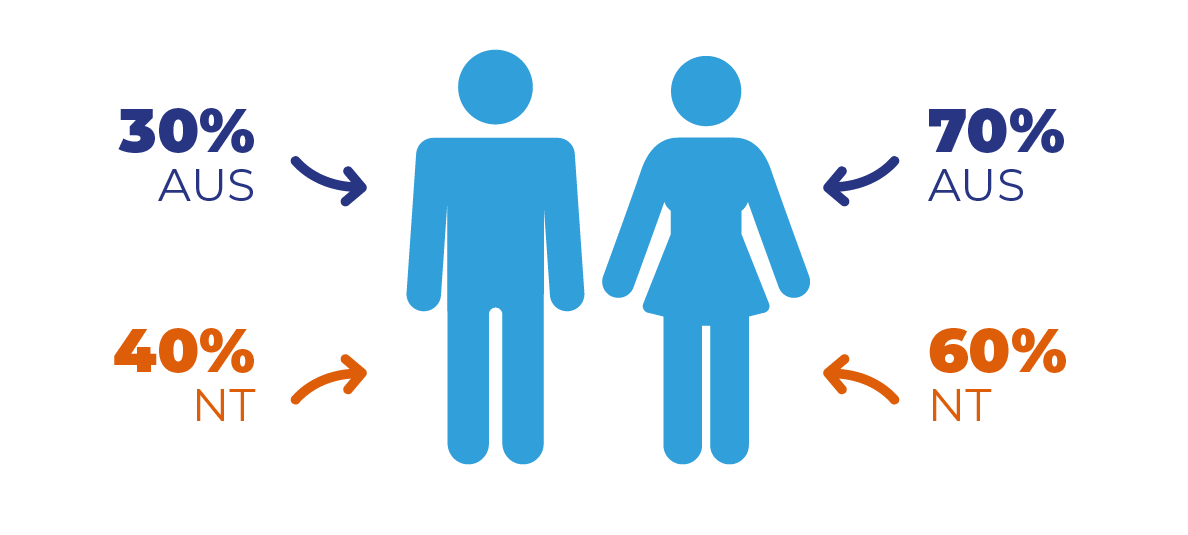
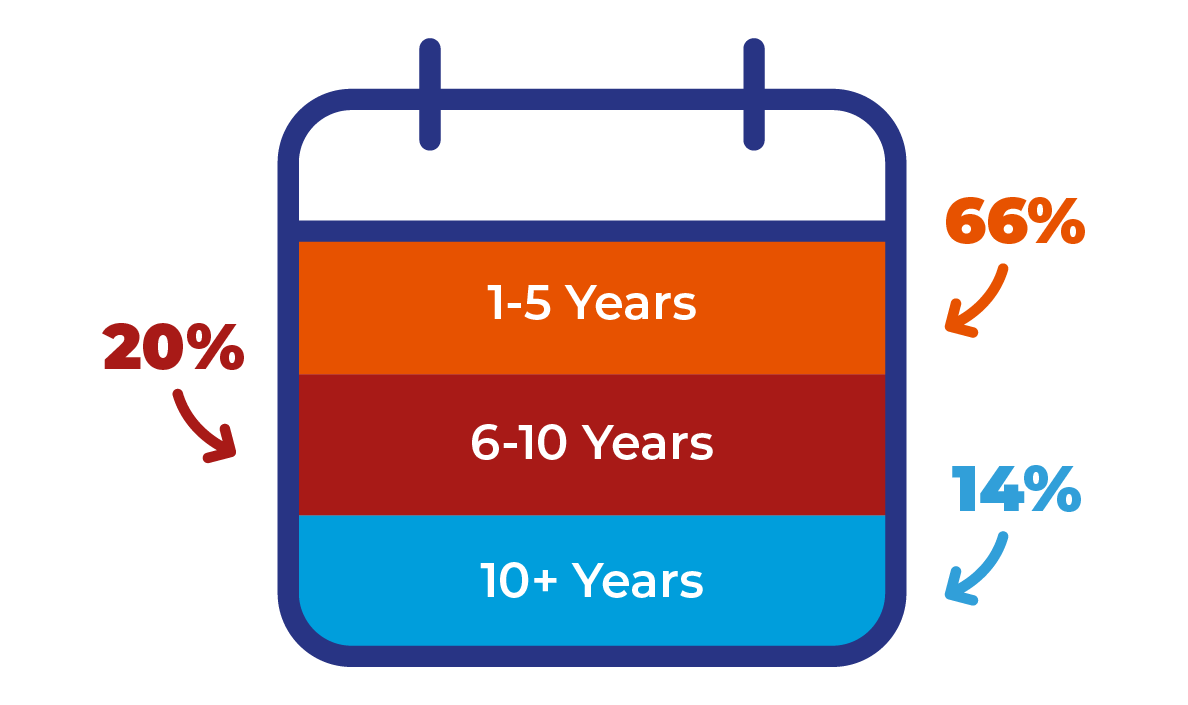
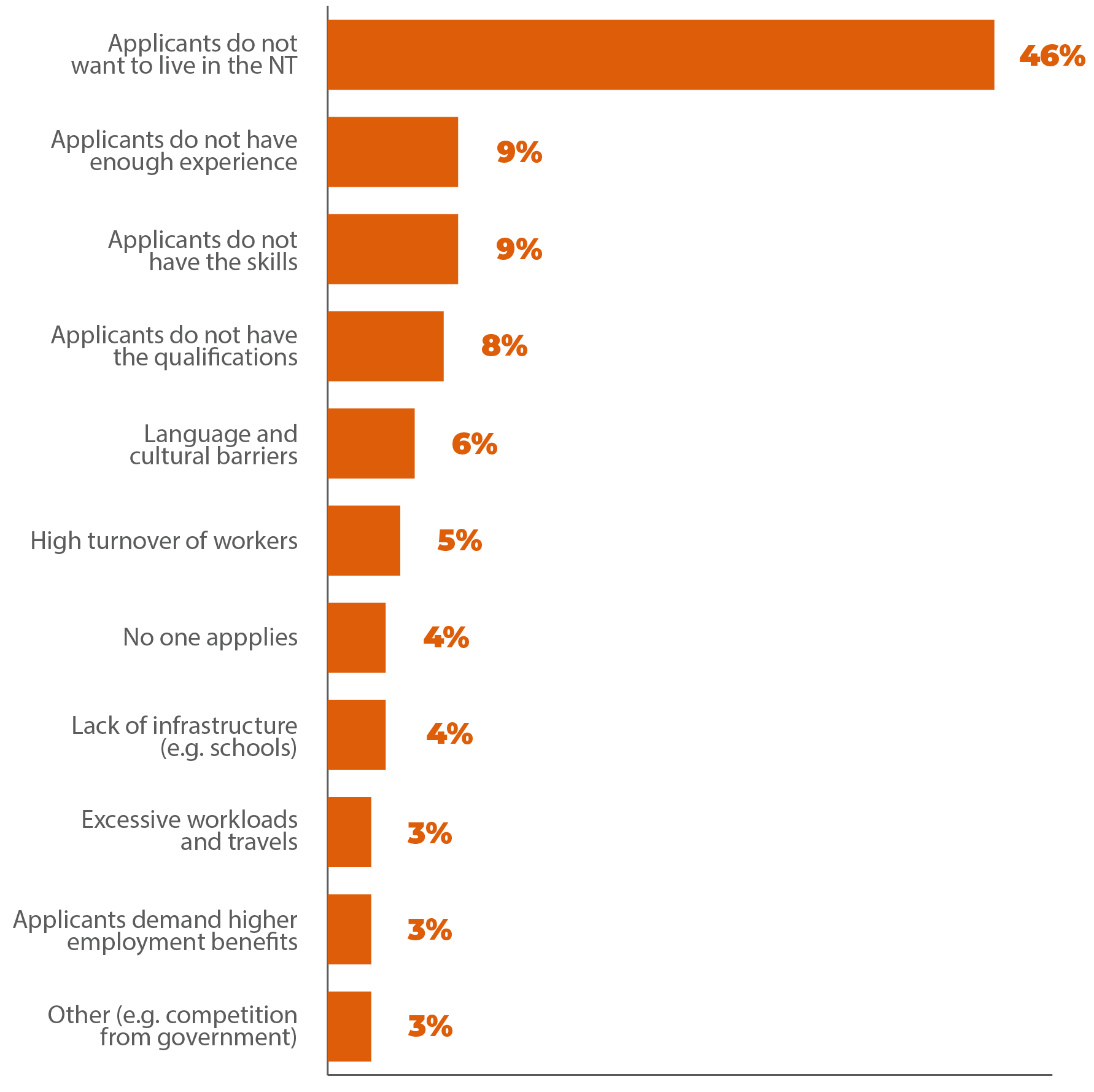
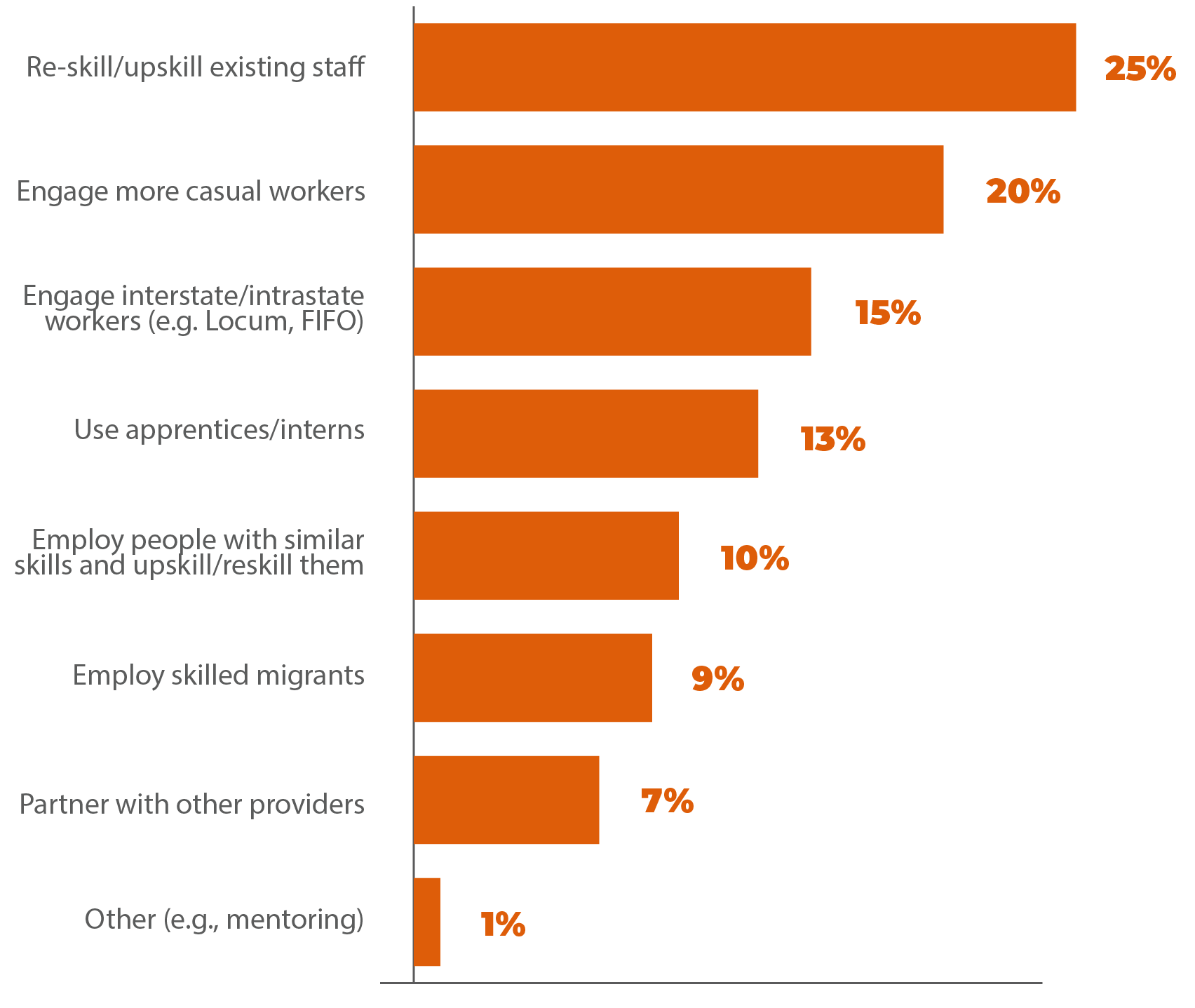
High workforce turnover: ISACNT’s consultation with service providers and industry associations revealed that staff turnover rates are higher for casual workers compared to permanent workers. Similarly, staff turnover was found to be higher in remote and very remote areas compared to urban Darwin. Competition between private and public providers is another contributor to staff turnover. For example, some stakeholders indicated the opening of the Howard Springs Quarantine Facility resulted in intense competition for disability workers between private providers and the government. Others also indicated the government’s ability to provide better conditions of services contributed to the loss of workers from the private to the public sector.
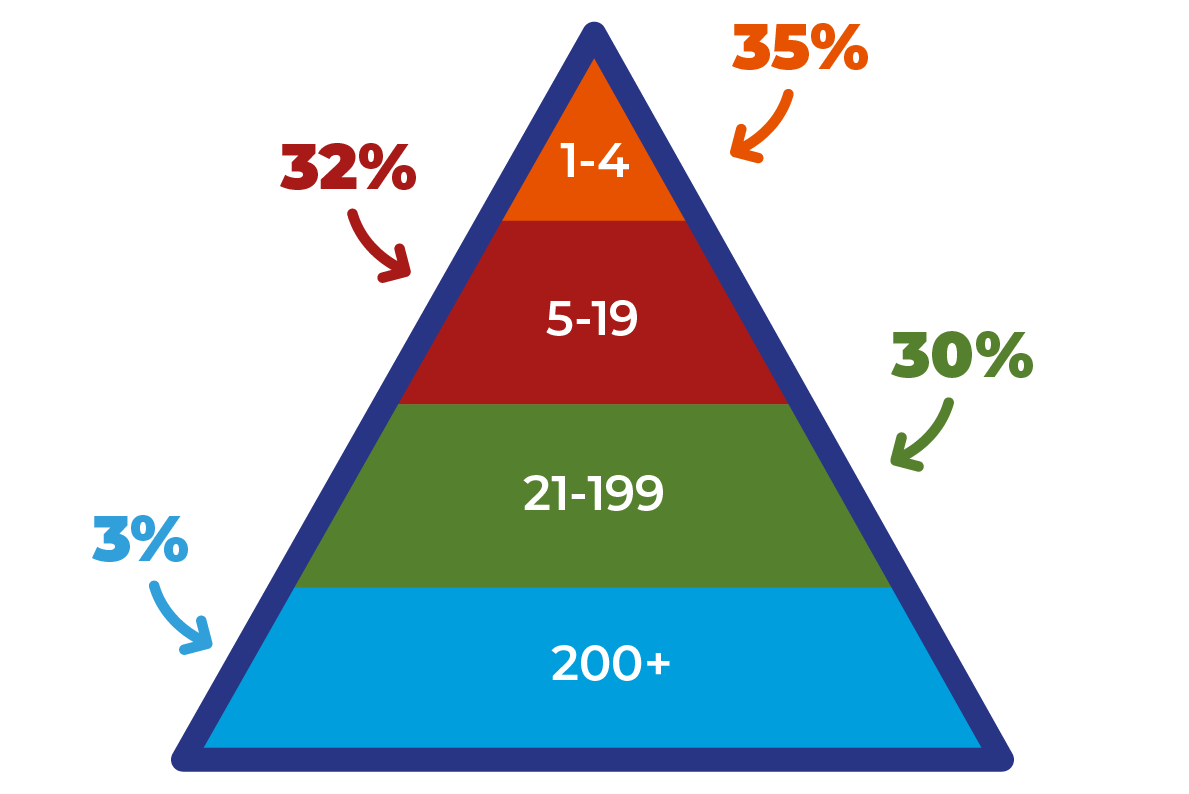
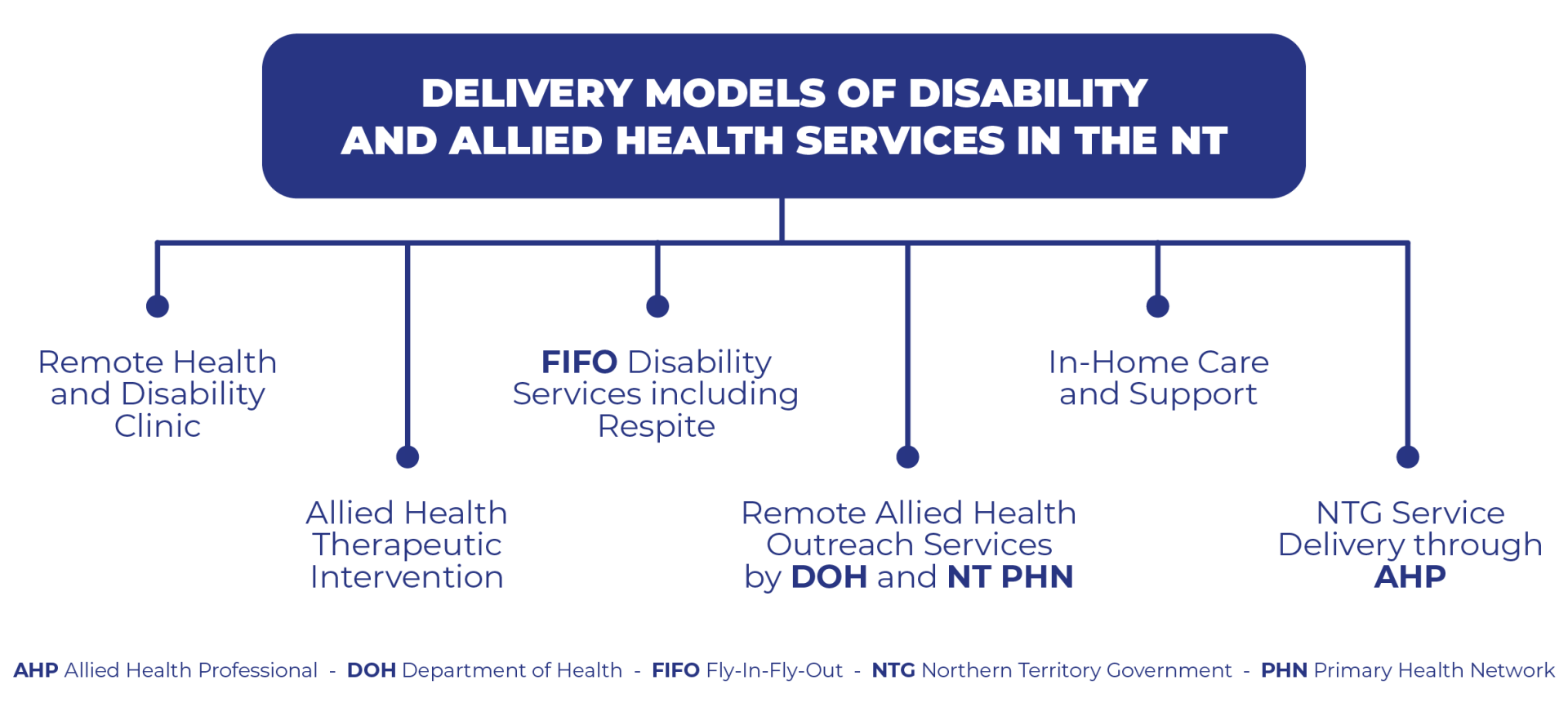
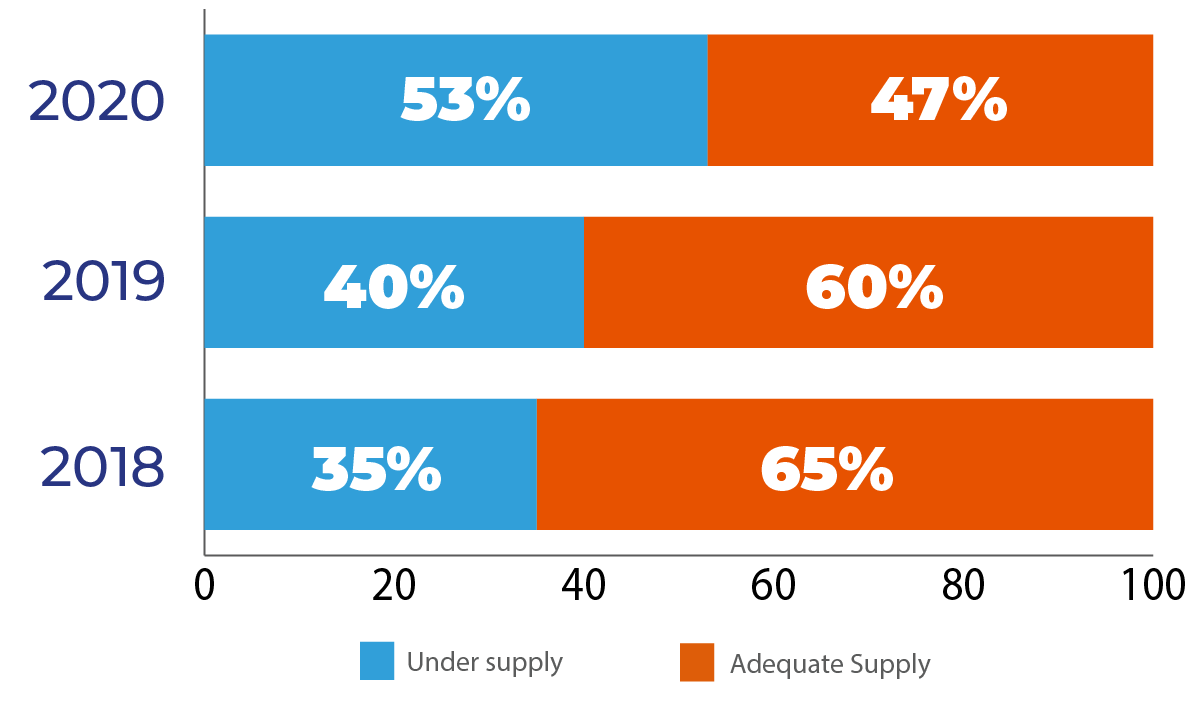
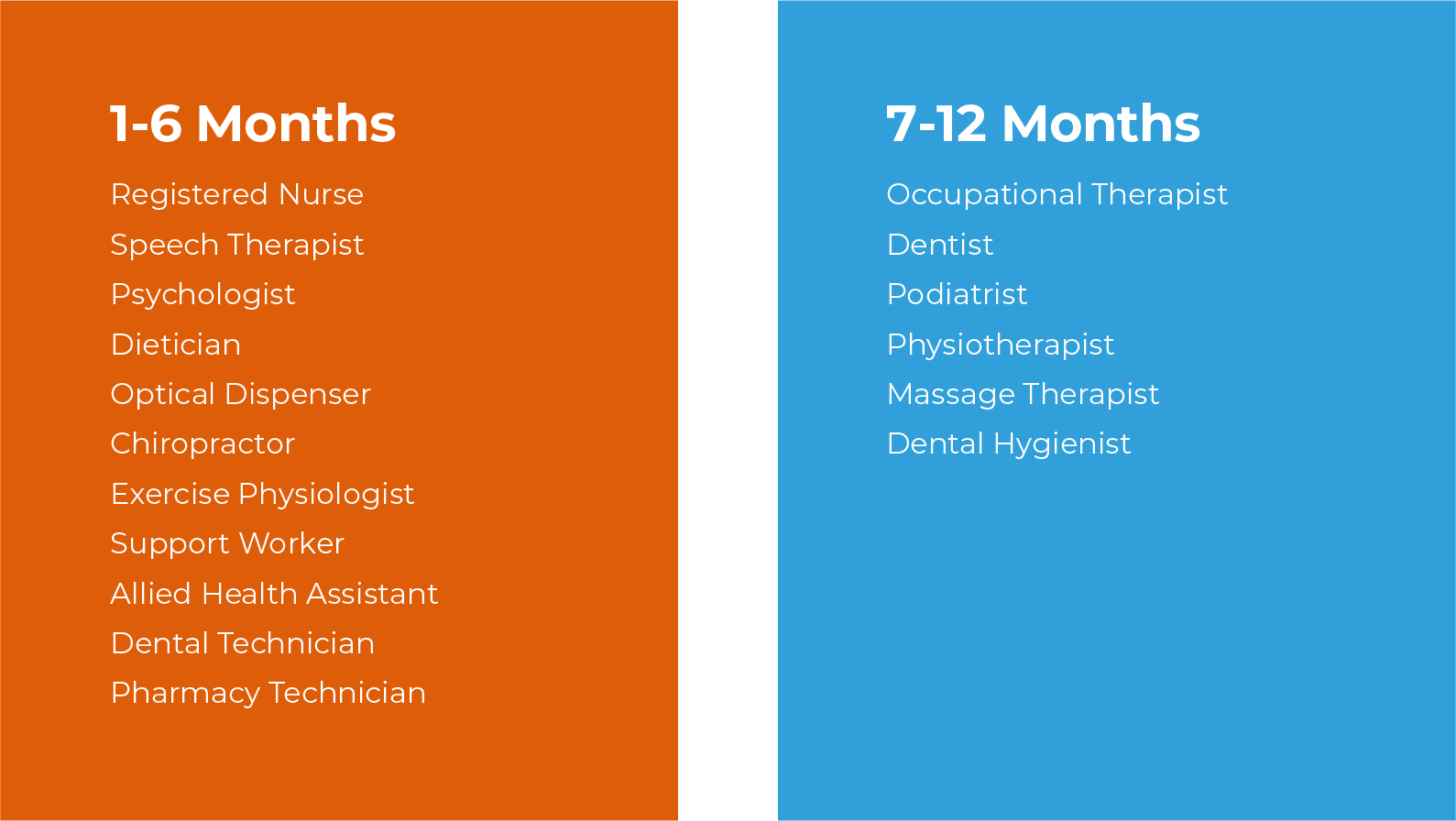
Recruitment and retention difficulties: Recruitment and retention of workers are becoming increasingly difficult in both the disability and allied health sub-sectors and across all regions of the NT. The recruitment and retention difficulties cut across all professions of allied health, often resulting in longer waiting times for participants as service demand exceeds the existing workforce and service supply. In the disability sub-sector, several providers stated that it was difficult to fill management roles, such as team leaders and support coordinators. This research also found that providers who are smaller in size found it more difficult to recruit suitable workers and retain them compared to larger ones. Many remote providers also expressed challenges retaining their workforce during the border closure as a result of the COVID-19 pandemic.
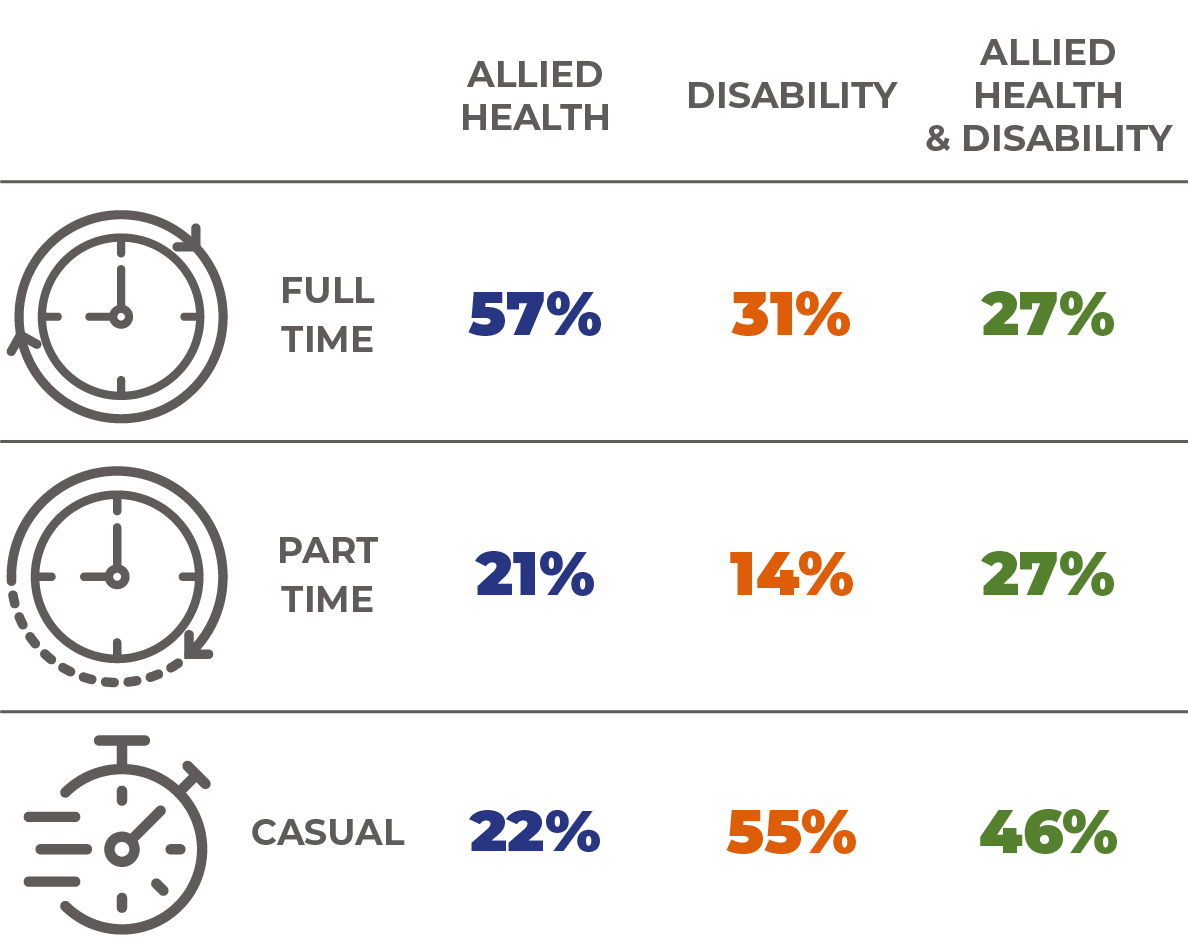
Rising workforce casualisation: The nature of the NDIS model of service delivery has led service providers to employ more casual workers. Casualisation of the workforce is more pronounced in the disability sub-sector compared to allied health. The rising casualisation of the disability sub-sector’s workforce often leads to many staff working less than full-time hours across multiple jobs while dealing with unstable rostering arrangements and constant shift changes. Such situations increase the risk of burnout, impacting workers themselves but also the patients.